Parasites take a huge toll on the health of humans and animals. But researchers may have found a way to turn patients with brain disorders and a common brain parasite into frenemies.
A new study published in Nature Microbiology has pioneered the use of a single-celled parasite, Toxoplasma gondiito inject therapeutic proteins into brain cells. The brain is very picky about what it lets in, including many drugs, which limits treatment options for neurological disorders.
As a professor of microbiology, I have dedicated my career to finding ways to kill dangerous parasites, such as ToxoplasmaI’m fascinated by the prospect that we might be able to use their weapons to treat other diseases.
Microbes as medicine
Ever since scientists realized that microscopic organisms can cause disease—what was called the 19th-century germ theory of disease—humanity has been searching for ways to keep infectious agents out of our bodies. Many people’s understandable aversion to germs can make the idea of modifying these microbial adversaries for therapeutic purposes seem counterintuitive.
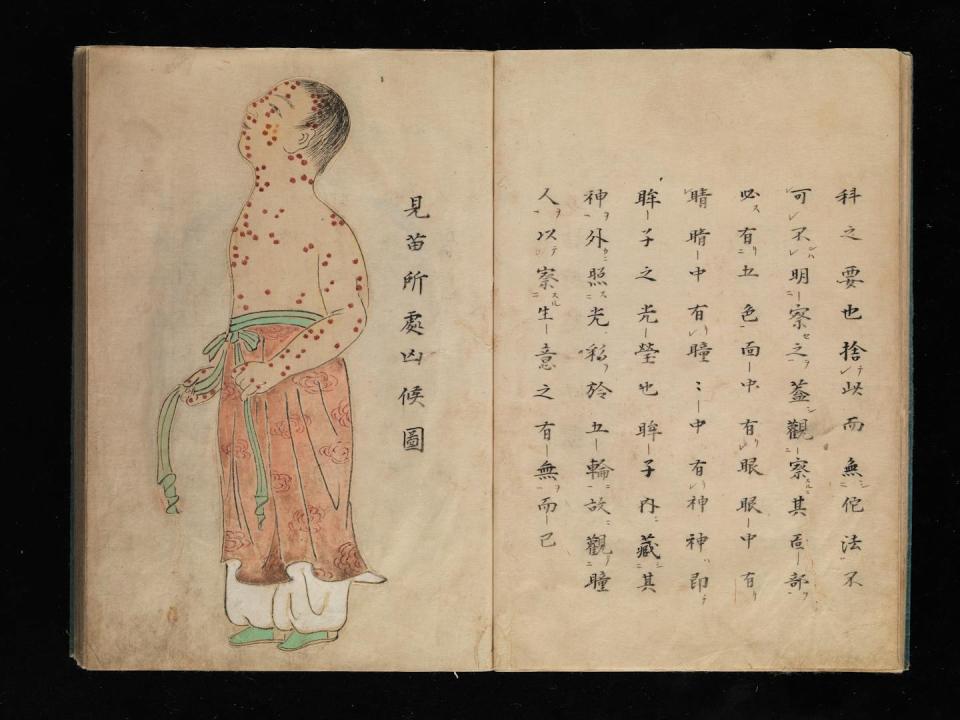
But preventing and treating disease by co-opting the microbes that threaten us has a history that long predates germ theory. As early as the 1500s, people in the Middle East and Asia noted that those lucky enough to survive smallpox were never infected again. These observations led to the practice of purposefully exposing an uninfected person to material from an infected person’s pus-filled sores—which, unbeknownst to them, contained weakened smallpox virus—in order to protect them from serious illness.
This vaccination concept has led to a flood of vaccines that have saved countless lives.
Viruses, bacteria and parasites have also developed many tricks to invade organs such as the brain and could be re-engineered to deliver drugs into the body. Such applications could include viruses for gene therapy and gut bacteria to treat a gut infection known as C.different.
Why can’t we just take a pill for brain diseases?
Pills provide a convenient and effective way to get medicine into the body. Chemical drugs such as aspirin or penicillin are small and are easily absorbed from the intestines into the bloodstream.
In contrast, biologics such as insulin or semaglutide are large, complex molecules that are vulnerable to being broken down in the stomach before they can be absorbed. They are also too large to pass through the intestinal wall into the bloodstream.
All drugs, especially biologics, have great difficulty entering the brain because of the blood-brain barrier. The blood-brain barrier is a layer of cells that lines the blood vessels of the brain and acts as a gatekeeper to prevent bacteria and other unwanted substances from entering neurons.
Toxoplasma offers delivery service to brain cells
Toxoplasma parasites infect all animals, including humans. Infection can occur in several ways, including ingesting spores released in the feces of infected cats or consuming contaminated meat or water. Toxoplasmosis in otherwise healthy people causes only mild symptoms, but can be serious in people with weakened immune systems and in a pregnant fetus.
Unlike most pathogens, Toxoplasma can cross the blood-brain barrier and enter brain cells. Once inside neurons, the parasite releases a series of proteins that alter gene expression in its host, which may be a factor in the behavioral changes it causes in infected animals and humans.
In a new study, a global team of researchers has hijacked the system Toxoplasma used to secrete proteins into its host cell. The team genetically engineered Toxoplasma to make a hybrid protein, by fusing one of its secreted proteins to a protein called MeCP2, which regulates gene activity in the brain — essentially giving MeCP2 a piggyback ride to neurons. Researchers found that the parasites secreted the MeCP2-protein hybrid into neurons grown in a petri dish, as well as into the brains of infected mice.
A genetic deficiency in MECP2 causes a rare brain development disorder called Rett syndrome. Gene therapy trials using viruses to deliver the MeCP2 protein to treat Rett syndrome are underway. If Toxoplasma deliver a form of MeCP2 protein into brain cells, it could provide another option for treating this currently incurable condition. It could also provide another treatment option for other neurological problems that arise from abnormal proteins, such as Alzheimer’s and Parkinson’s disease.
The long road ahead
The road from the lab to the hospital is long and full of obstacles, so don’t expect any constructed solutions. Toxoplasma soon in the clinic.
The obvious complication when using Toxoplasma for medical purposes is that it can cause a serious, lifelong infection that is currently incurable. Infecting someone with Toxoplasma can damage vital organ systems such as the brain, eyes and heart.
However, worldwide, one-third of people currently wear a Toxoplasma in their brains, apparently without incident. New studies have linked the infection to an increased risk of schizophrenia, anger disorder and recklessness, suggesting that this silent infection may make some people more susceptible to serious neurological problems.
The widespread prevalence of Toxoplasma infections can also be another complication, as it disqualifies many people from using it for treatment. Since the billions of people who already carry the parasite have developed immunity to future infections, therapeutic forms of Toxoplasma would be quickly destroyed by their immune systems once injected.
In some cases the benefits of using Toxoplasma as a drug delivery system may outweigh the risks. Developing benign forms of this parasite could produce the proteins patients need without damaging the organ – the brain – that defines who we are.
This article is republished from The Conversation, a nonprofit, independent news organization that brings you facts and reliable analysis to help you understand our complex world. It was written by: Bill Sullivan, Indiana University
Read more:
Bill Sullivan receives funding from the National Institutes of Health.