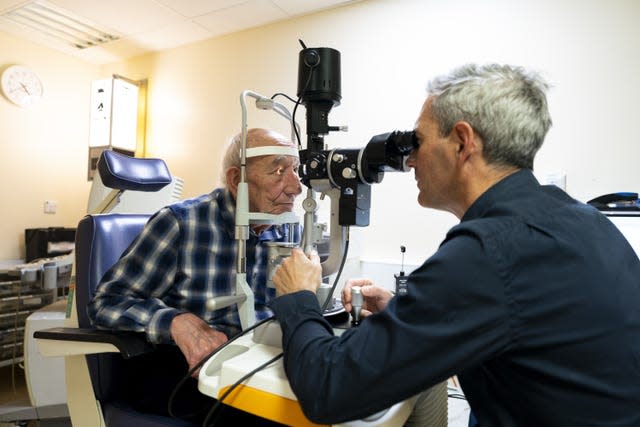
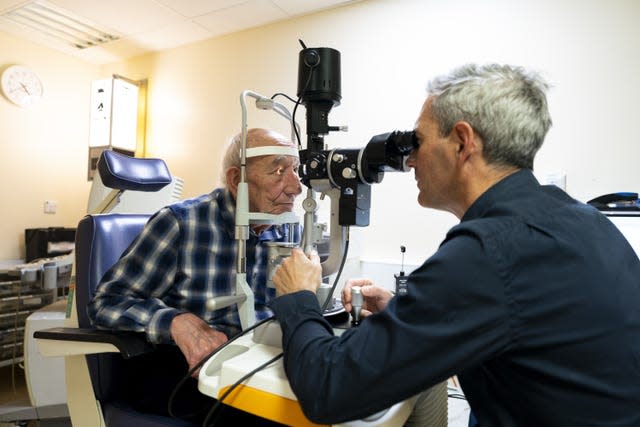
A 91-year-old man has made history by becoming the first patient in England to receive an artificial cornea.
Cecil Farley had to wait a year for sight-saving surgery after a human cornea transplant failed, but his surgeon offered him the chance to skip the queue by using an artificial cornea transplant.
Medics hope that the new artificial corneas could one day reduce the need for human cornea donations.
Frimley Health NHS Foundation Trust consultant ophthalmologist Thomas Poole told the PA news agency that the use of artificial corneas is a “major advance for patient care”.
The new product replaces the inner part of the cornea.
Likened to a contact lens, it is surgically attached to the eye with a single stitch and set in place with a gas bubble.
Mr Farley, known to his friends as John, said the transplant has allowed him to continue seeing his 83-year-old wife Elizabeth.

He had no vision in his right eye, but his vision has slowly improved since the procedure, which took place in February.
Mr Farley, from Chobham in Surrey, had had problems with his eyes for about 15 years.
Medics from Frimley offered the procedure, a type of corneal implant called endothelial keratoplasty, which involves removing the abnormal inner lining of the cornea and replacing it with an artificial cornea, rather than a donated human cornea.
“I can still see my wife after 63 years of marriage, we can just carry on as normal and live life as fully as possible,” Mr Farley told PA.
“It makes your life fuller when your eyes are working properly – you don’t realize how debilitating it is until it happens to you.”
The retiree, who used to own a flooring company, said that once his eyesight is fully restored he wants to do practical tasks such as repairing a watch, but for now he is content to ‘move around’.
“It has made a big difference to my vision. It was very blurry and I couldn’t make out a face. Now I can see better with it, the brighter the light, the better. It’s slow; they said it could take up to a year,” Farley said.
The cornea is the clear outer layer at the front of the eyeball.


When a cornea becomes damaged due to injury or disease, it may become less transparent or its shape may change.
This can prevent light from reaching the retina at the back of the eye, causing the image sent to the brain to be distorted or unclear.
A corneal transplant can be performed to improve vision, relieve pain, and treat serious infections or damage.
Corneal transplants usually come from deceased donors.
Mr Poole and his colleague Hanbin Lee have successfully fitted four patients with artificial corneas over the past two months and initial results have shown an improvement in vision.
“It’s a major advance for patient care, and it will be a great opportunity for some patients who can’t wait too long or have other eye co-morbidities,” Mr Poole said.
“We now have a very long waiting list for a human cornea, which we have been using with great success for years. The problem is that if you have patients whose eyes are deteriorating, you can’t get a human cornea for more than a year.
“There are risks associated with being on a waiting list with an unwell eye; There are risks if you don’t do anything very well, such as contracting an infection.
“One of the beauties of (the artificial cornea) is that it’s not human tissue, so the body doesn’t try to reject it.
“Looking to the future, I think this could eventually replace human corneas in certain types of corneal transplant patients. In maybe ten or twenty years, this could become the norm where we don’t need a human cornea, and we can just take one out of the box.”
Mr Poole added: “I’ve just booked three people for this. All three have had failed transplants in the past, and all three have a one-year waiting list. We can just take it out of the closet. I can do it in the next few months, instead of waiting a year.
“The three patients I mentioned today are a good example of this: they now no longer need a human cornea, so that will take the pressure off the waiting lists.”
Speaking about Mr Farley’s case, Mr Poole said: “He has had a failed corneal transplant and his cornea – the clear window at the front of the eye – was cloudy and boggy.
‘He had had many operations and my concern was that we would be able to use a human cornea for him again, but that puts him at great risk of failure… he was almost reaching the last hope.
“John had this artificial cornea fitted in February and clinically we can already see that his cornea is so much less swollen than it was, that it is becoming better shaped and clearer. Week after week he says it gets a little better each time.
Mr Poole added: “I had a very frank conversation with him earlier and I said, ‘Look, your transplant has failed, you’re back on the waiting list. Because your other eye sees reasonably well, you are not high on the waiting list and you may have to wait another year.’
“He’s in his 90s now and said, ‘I just can’t wait that long. Is there anything else?’ And so this came to mind: I had just read a publication about very good reports on this artificial graft and it got me thinking: maybe we can use this for John.
NHS England national medical director Professor Sir Stephen Powis said: “The use of artificial corneal transplants is an exciting and innovative step forward in eye care, which has the potential to benefit many patients who need treatment to improve or improve their vision. to recover.
“It could provide an additional treatment option for people waiting for donated transplants, and it is heartening to hear that patients like Cecil are already benefiting from its use.”


According to the latest available figures, around 4,719 corneas were supplied to NHS Blood and Transplant Eye Banks in 2022/23 and there were 3,529 transplants.
In the past, some potential organ donors have said they were willing to donate organs, including hearts, livers and kidneys, but chose not to donate their corneas.
Kyle Bennett, assistant director for tissue and eye services at NHS Blood and Transplant, said: “We understand that people often attach more emotion and symbolism to the eyes than to other parts of the body, and may therefore be reluctant to agree with cornea donation.
“However, agreeing to this form of donation, even if solid organ donation may not be possible, means that light can come after darkness for the thousands of people in need of a corneal transplant.
“One donor alone can help up to ten people restore or improve their vision so they can see their friends and family clearly again.
“We are so grateful to everyone who agreed to donate their corneas after their death and restored or improved the vision of 3,259 people through corneal transplants last year.”
The new artificial cornea, called EndoArt, was created by ophthalmic medical device company EyeYon Medical.
So far, only 200 have been implanted worldwide, including Mr Farley’s.
“EndoArt is the first artificial endothelial layer, a promising treatment for select eyes with chronic corneal edema,” said Charles Holmes, the company’s Chief Commercial Officer.
“EndoArt represents a new hope for patients suffering from chronic corneal edema as an alternative to human tissue.”