Embryonic development, also called embryogenesis, is a cornerstone in understanding the origins of life. But studying this marvel of complex and layered biological processes in humans faces significant challenges. Early stage human embryos are difficult to obtain. Then there are ethical issues surrounding its use. This has made it difficult for scientists to understand early human development.
However, advances in genetic engineering and molecular and cellular biology have catalyzed the rise of synthetic embryology, a subfield dedicated to replicating and studying embryonic development in a petri dish using human stem cells. By providing new tools to investigate the enigmatic earliest stages of human development, synthetic embryology can help researchers overcome the challenges of using real human embryos.
As a reproductive and developmental biologist, I develop stem cell models for embryogenesis. These new models can also help researchers better understand the conditions that affect human reproduction and development, as well as maternal and fetal health, potentially leading to new therapies.
Creating human embryos from stem cells
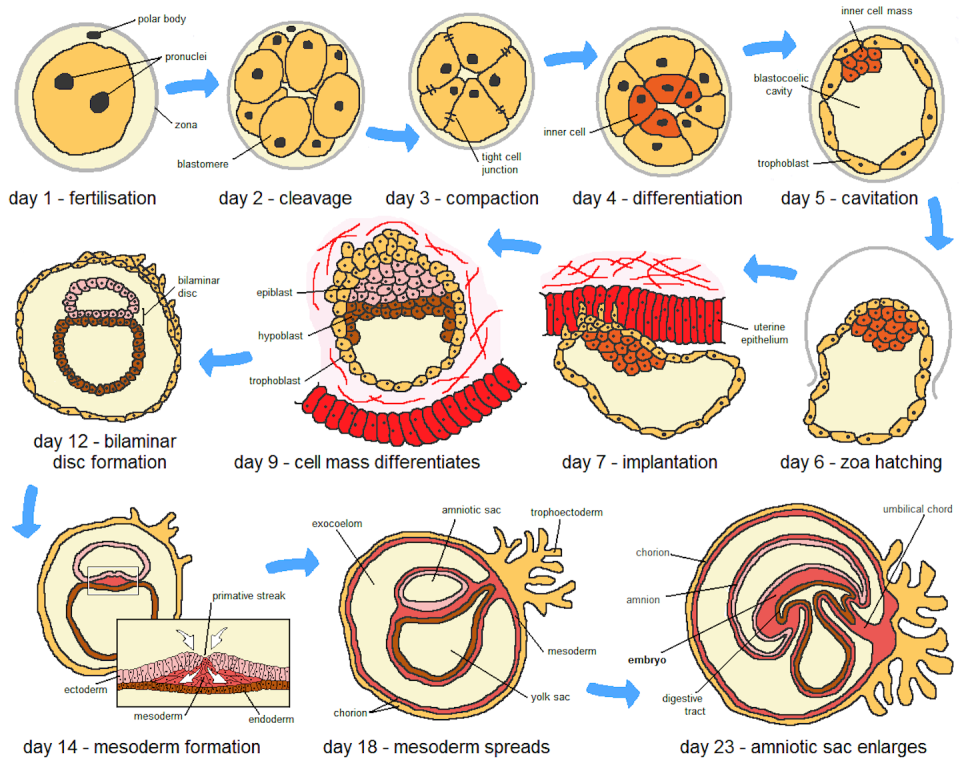
Embryogenesis begins with the fertilization of an egg. This causes the egg to divide rapidly into embryonic cells that soon form an inner cell mass that eventually develops into the fetus and an outer layer of cells that will give rise to the placenta.
When implanted in the uterus, the inner cell mass develops into the three layers that will create all tissues and organs of the human body. At the same time, the placenta begins to form as the embryo attaches to the uterine wall, a crucial step for the connection between mother and fetus. This attachment allows the transfer of nutrients, oxygen and waste products between mother and fetus.
Synthetic embryology artificially mimics these developmental stages using human pluripotent stem cells derived from human embryos or induced from adult human cells. Like early embryonic cells, these cells have the ability to develop into any type of cell in the human body. In carefully designed laboratory environments, researchers can coax these cells to form multicellular structures that mimic various embryonic stages of development, including early organ formation.
Researchers created the first human embryo model from embryonic stem cells in 2014. Also called a gastruloid, this groundbreaking model captured important aspects of early human development and showed that scientists can direct pluripotent stem cells to form patterned layers that reflect the three germ layers and the outermost layers of the embryo.
Gastruloids are easy to replicate and measure when studying early events in development. These 2D gastruloids can also help researchers accurately identify and image embryonic cells. However, this model lacks the complex 3D structure and spatial cell interactions seen in natural embryogenesis.
Advances in human embryo models
Since the first gastruloid, the field has made significant progress.
Over the years, several models have managed to replicate different facets of human embryogenesis, such as amniotic sac development, germ layer formation, and body plan organization. Researchers have also developed organ-specific models of early organ development, such as a model that captures key events in neural development and fetal lung organoids that mimic the process of lung formation.
However, none of these models fully captures the entire process of a single cell type developing into the complete structure of an entire embryo.
A major breakthrough occurred in 2021 when several research groups successfully used human pluripotent stem cells with higher developmental potential to create blastoids, which resemble early-stage embryos before implantation. Blastoids form in a similar way to human embryos, starting from just a few cells that multiply and organize themselves.
The developmental and structural similarity of blastoids to embryos makes them useful for studying the first steps of embryo formation, especially before they attach to the uterus. Blastoids can attach to laboratory dishes and undergo further growth. They can also mimic the implantation of embryos in the uterus by integrating with maternal endometrial cells and developing into later embryonic stages after implantation.
Recently, researchers have successfully created more complex models in the laboratory that mimic what happens after embryos attach to the uterus. Two research teams used specially engineered cells to create structures similar to those of human embryos about a week after implantation. These models are also able to form the cells that eventually turn into sperm and eggs in humans, mirroring what happens in natural development.
Another research group also managed to create a similar model from pluripotent stem cells, without having to genetically manipulate them. This model is able to mimic even later stages of development and the beginning of nervous system formation.
Choosing the right models
In the evolving field of synthetic embryology, no single model can perfectly capture all aspects of embryogenesis. The goal, then, is not to play God and create life in a petri dish, but rather to expand our understanding of ourselves. This goal underlines the importance of carefully choosing the model that best fits the specific research objectives at hand.
For example, my previous work focused on chromosomal abnormalities in early human development. Aneuploidy, or cells with an abnormal number of chromosomes, is a leading cause of pregnancy loss. But scientific knowledge about how these abnormal cells affect pregnancy and fetal development is very limited.
Because gastruloids can effectively model these aspects of early development, this system could be ideal for studying aneuploidy in early development. This allows researchers to accurately monitor and analyze how aneuploid cells behave and how they influence developmental processes.
Using this model, my team and I discovered that cells with chromosomal abnormalities are more likely to develop into cells in the placenta and are likely to be eliminated during fetal cell development. This finding provides significant insight into why babies with normal chromosome numbers can be born healthy even if aneuploidy is detected during pregnancy. Such discoveries are valuable for improving diagnostic and prognostic methods in prenatal care.
Future models that more completely replicate embryonic structures and better reflect biological events will not only advance understanding of the fundamentals of early development but also have great potential in addressing clinical problems. Researchers can use them to model diseases and develop drugs for early life or genetic conditions. These models are also invaluable for studying tissue formation in regenerative medicine. Creating embryo models from a patient’s own cells could also allow researchers to study the genetics of development and help personalize treatments.
The key to progress in the field of synthetic embryology is an unwavering adherence to ethical standards and regulations. Crucially, these embryo models are neither synthetic nor real embryos. The International Society for Stem Cell Research strictly prohibits the transfer of these embryo models into the uterus of any human or animal. Although these models mimic certain characteristics of early stages of development, they cannot and will not develop into the equivalent of a human baby after birth. Basing research on sound justifications and oversight will help ensure that scientific research into the structure of life is conducted with the utmost respect and responsibility.
By embracing the complexity and potential of synthetic embryology, researchers are on the cusp of a new era in biological understanding and ready to unravel the mysteries of life itself.
This article is republished from The Conversation, an independent nonprofit organization providing facts and trusted analysis to help you understand our complex world. It was written by: Min Yang, University of Washington
Read more:
Min (Mia) Yang receives funding from the University of Washington